Vera Regina Cerceau1, Hudson Azevedo Pinheiro1, Marina Cerceau Silva1, Marina Morato Stival2
1Multidisciplinary Residency Program in Adult and Elderly Health (ESP/FEPECS/SESDF), Brasília, Federal District, Brazil
2University of Brasília (UnB), Brasília, Federal District, Brazil
Received: May 23, 2025; Accepted: May 28, 2025.
Correspondence: Vera Regina Cerceau, vrcerceau@gmail.com
How to cite
Cerceau VR, Pinheiro HA, Silva MC, Stival MM. Risk of dysphagia, sarcopenia and quality of life in elderly women. Geronto Bras. 2025;1(1):70-84. doi:10.62827/gb.v1i1.0007
Abstract
Introduction: With population aging, changes in the general state of the individual may occur, among these changes are sarcopenia, dysphagia and malnutrition. Among elderly women this may occur more pronouncedly due to post-menopausal hormonal changes. These changes may compromise the Quality of Life of the age group of 60 years or older. Objective: Sarcopenia can occur in human aging and, when associated with conditions such as dysphagia, can have a negative impact on quality of life. The objective was to evaluate the association of sarcopenia and dysphagia with the Quality of Life of elderly women. Methods: Cross-sectional study carried out with 258 elderly women treated at the geriatric outpatient clinic of the SUS. Clinical characteristics, risk of dysphagia by the Eating Assessment Tool (EAT-10), sarcopenia and quality of life by the EuroQol five-dimensional questionnaire (EQ-5D) were evaluated. Linear regression was used to determine the prediction model for Quality of Life. Results: The median age of the women was 73 years, sedentary, edentulous, with urinary incontinence and polypharmacy. It was found that the worst Quality of Life (QoL) scores were present in elderly women with sarcopenia, risk of dysphagia (osteoporosis) and urinary incontinence. A high prevalence of edentulism and urinary incontinence was observed. There was no interference in the quality of life of the elderly women investigated, but there was an impact on those who presented urinary incontinence and risk of dysphagia. Conclusion: Elderly women with risk of dysphagia and urinary incontinence had worse Quality of Life scores, mainly in the dimensions Pain/discomfort and Mobility. No association was observed between sarcopenia and QoL.
Keywords: Aged; Deglutition Disorders; Sarcopenia; Urinary Incontinence; Quality of Life.
Resumo
Risco de disfagia, sarcopenia e qualidade de vida em mulheres idosas
Introdução: Com o envelhecimento populacional podem ocorrer alterações no estado geral do indivíduo, dentre estas alterações estão a sarcopenia, a disfagia e desnutrição. Entre as mulheres idosas isso pode ocorrer de forma mais acentuada devido as alterações hormonais pós-menopausa. Estas alterações podem comprometer a Qualidade de vida da faixa etária de 60 anos ou mais. Objetivo: A sarcopenia pode ocorrer no envelhecimento humano e, quando associada a condições como a disfagia, pode ter impacto negativo na qualidade de vida. Avaliou-se a associação da sarcopenia e da disfagia com a Qualidade de Vida de mulheres idosas. Métodos: Estudo transversal realizado com 258 mulheres idosas atendidas no ambulatório de geriatria do SUS. Foram avaliadas características clínicas, risco de disfagia pelo Eating Assessment Tool( EAT-10), sarcopenia e qualidade de vida pelo EuroQol five-dimensional questionnaire (EQ-5D). A regressão linear foi utilizada para determinar o modelo de predição de Qualidade de Vida. Resultados: A mediana de idade das mulheres foi de 73 anos, sedentárias, edêntulas, com Incontinência urinária e polifarmácia.Verificou-se que os piores escores de Qualidade de Vida (QV) estavam presentes nas mulheres idosas com sarcopenia, risco de disfagia osteoporose) e incontinência urinária.Foi observada alta prevalência de edentulismo e incontinência urinária.Não houve interferencia na qualidade de vida das idosas investigadas, mas houve impacto nas que apresentaram incontinencia urinaria e risco de disfagia. Conclusão: Mulheres idosas com risco de disfagia e incontinência urinária apresentaram piores escores de Qualidade de Vida, principalmente nas dimensões Dor/desconforto e Mobilidade. Não se observou associação entre sarcopenia e QV.
Palavras-chave: Idosos; Transtornos da Deglutição; Sarcopenia; Incontinência Urinária; Qualidade de Vida.
Resumen
Riesgo de disfagia, sarcopenia y calidad de vida en mujeres mayores
Introducción: Con el envejecimiento poblacional pueden presentarse cambios en el estado general del individuo, entre estos cambios se encuentran la sarcopenia, la disfagia y la desnutrición. Entre las mujeres mayores, esto puede ocurrir de manera más pronunciada debido a los cambios hormonales posmenopáusicos. Estos cambios pueden comprometer la calidad de vida de las personas de 60 años o más. Objetivo: La sarcopenia puede ocurrir durante el envejecimiento humano y, cuando se asocia con afecciones como la disfagia, puede tener un impacto negativo en la calidad de vida. El objetivo fue evaluar la asociación de la sarcopenia y la disfagia con la Calidad de Vida de mujeres mayores. Métodos: Estudio transversal realizado con 258 mujeres mayores atendidas en el ambulatorio geriátrico del SUS. Se evaluaron las características clínicas, el riesgo de disfagia mediante el Eating Assessment Tool (EAT-10), la sarcopenia y la calidad de vida mediante el cuestionario de cinco dimensiones EuroQol (EQ-5D). Se utilizó regresión lineal para determinar el modelo de predicción de calidad de vida. Resultados: La mediana de edad de las mujeres fue de 73 años, sedentarias, edéntulas, con incontinencia urinaria y polifarmacia. Se encontró que los peores puntajes de Calidad de Vida (CV) estaban presentes en mujeres mayores con sarcopenia, riesgo de disfagia (osteoporosis) e incontinencia urinaria. Se observó una alta prevalencia de edentulismo e incontinencia urinaria. No hubo interferencia en la calidad de vida de las ancianas investigadas, pero sí impacto en aquellas que presentaron incontinencia urinaria y riesgo de disfagia. Conclusión: Las mujeres mayores con riesgo de disfagia e incontinencia urinaria presentaron peores puntuaciones de Calidad de Vida, especialmente en las dimensiones Dolor/malestar y Movilidad. No se observó asociación entre la sarcopenia y la calidad de vida.
Palabras-clave: Anciano; Trastornos de Deglución; Sarcopenia; Incontinencia Urinaria; Calidad de Vida.
Introduction
Population aging imposes specific demands on health systems and the scientific community, which seek to understand and monitor the epidemiological profile of elderly populations worldwide, as well as to respond to the needs and demands concerning quality of life (QoL). To this end, parameters that interact positively and/or negatively with QoL are used, aiming to mitigate biopsychosocial challenges and enhance the physiological and intrinsic aspects of the elderly’s physical, mental, and functional abilities, considering the environment in which they live [1,2,3].
Among the challenges related to the organic domain, particularly to intrinsic and physiological aspects of aging, sarcopenia refers to the progressive and generalized decline of the musculoskeletal system, characterized by a mandatory decrease in muscle mass, associated with reduced muscle strength and/or physical performance. This condition deserves attention because there are no clinical guidelines for its control, and its cost management has become particularly important due to a significant increase in cases. Therefore, interventions aiming to maintain and improve QoL are needed, as the disease imposes high personal and societal costs [4,5].
In Brazil, the prevalence of sarcopenia ranges from 4.8% to 62.0%, influenced by the assessment methodologies used, the characteristics of the population under study, and the definitions applied in different studies [5]. Furthermore, the condition has a higher prevalence among women than men (16.1% vs. 14.4%) as observed in studies conducted in countries like Brazil, Japan, South Korea, the United States, Taiwan, and the United Kingdom [5]. Sarcopenia is generally associated with non-communicable chronic diseases, cognitive deficits, advanced age, malnutrition/nutritional deficiencies, physical inactivity, smoking, polypharmacy, and is prevalent among bedridden and institutionalized elderly individuals [6,7].
In relation to other medical conditions, the report from the Japanese Society of Dysphagia Rehabilitation highlighted the correlation between sarcopenia and dysphagia, a swallowing disorder, through two distinct and cyclical patterns: whole-body sarcopenia/malnutrition followed by dysphagia, and dysphagia followed by whole-body malnutrition/sarcopenia [8,9]. Dysphagia is a condition whose prevalence in elderly people ranges from 10% to 60%, increasing by an average of 3% with each year of life [10,11,12,13].
When associated, these conditions can negatively impact the QoL of elderly individuals, particularly women. According to the World Health Organization (WHO), QoL is the individual’s perception of their position in the sociocultural context in which they live, in relation to their goals, expectations, and concerns. Thus, QoL is directly associated with the individual’s ability to perform social roles, psychological well-being, adaptation, and functioning within social groups [14].
The results of this study may contribute a theoretical framework and empirical evidence for the scientific development of this subject, with a focus on QoL, and highlight the lack of literature on the domains affected by sarcopenia [15]. In this context, considering population aging, the prospect of increased life expectancy, and the potential of sarcopenia to affect the QoL of elderly individuals, with dysphagia being a condition associated with this disease, the present study aimed to evaluate the association of sarcopenia and dysphagia with the QoL of elderly women.
The objective of this study was to evaluate the association of sarcopenia and dysphagia with the quality of life of elderly women
Methods
This was a cross-sectional study with a quantitative approach, conducted with elderly women from a reference center in Geriatrics and Gerontology of the Health Department of the Federal District. The research was approved by the Research Ethics Committee of the Ceilândia School of the University of Brasília (CAEE 45969821.9.0000.8093). All participants received information about the study according to Resolutions No. 466/2012 and No. 510/2016 of the National Health Council and signed the Informed Consent Form (ICF).
Data Collection Procedures
Convenience sampling was used, with the following inclusion criteria: female sex and age ≥60 years; being followed up at the unit; and completing all assessments proposed in the research. Exclusion criteria were adopted based on the belief that these conditions present higher risks of malnutrition, dysphagia, and sarcopenia: patients with severe dementia, sequelae of stroke, Parkinson’s disease; those with amputated limbs, pacemakers, bedridden, or on alternative feeding routes. Thus, 258 elderly women were included between September 2021 and February 2022. Assessments were carried out in a private space in the outpatient clinic.
Initially, after agreeing to participate and signing the ICF, a structured interview was conducted to investigate the following variables: use of continuous medication, comorbidities, edentulism, urinary incontinence, and sedentary lifestyle, which were self-reported and confirmed through the Health Department’s electronic medical records.
To assess cognition, the Mini-Mental State Examination (MMSE) was used. It consists of dichotomous items with a maximum score of 30 points. The following cut-off scores for cognitive impairment were adopted: illiterate <21; 1–5 years of education <24; 6–11 years <26; 12 or more years <27 [16]. Elderly women with severe cognitive impairment that prevented test execution were excluded.
Sarcopenia was assessed using the criteria of the European Working Group on Sarcopenia in Older People, revised (EWGSOP2) [4].
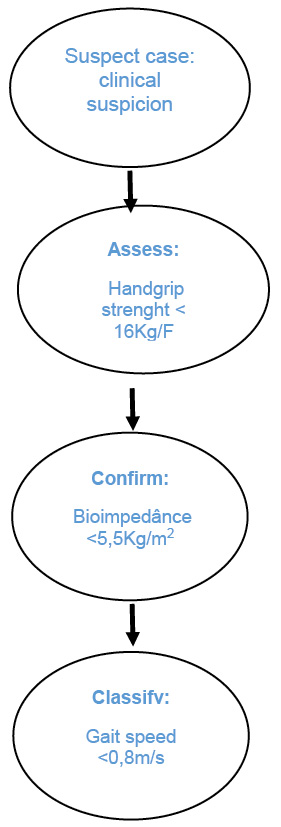
Source: the authors.
Figure 1 - Algorithm for identifying elderly women with sarcopenia according to the European Working Group of Sarcopenia in Older People revised (EWGSOP2)
Handgrip strength was measured with a SAEHAN® hydraulic dynamometer, using the dominant hand with three attempts. A mean value <16Kg/F was considered the cut-off [17]. According to EWGSOP2, low handgrip strength is a strong predictor of poor outcomes such as prolonged hospitalization, increased functional limitations, worse health, and even mortality [4].
Women without pacemakers were advised to follow specific protocols before bioimpedance analysis (BIA): fasting, no exercise in the last 24 hours, light clothing, removal of all metal items, no diuretics, and emptying the bladder. Body composition was assessed using the InBody® model 270 device. Appendicular Skeletal Muscle Mass (ASM) was calculated by summing muscle mass from upper and lower limbs [18].
Gait speed, which determines sarcopenia severity, was measured by asking participants to walk five meters on a flat surface. Speed <0.8m/s was considered indicative of severe sarcopenia [4].
Dysphagia risk was identified using the EAT-10, a self-assessment tool with 10 items covering functional (3), emotional (3), and physical (4) domains. A score of ≥3 was considered indicative of risk [19].
Nutritional risk was assessed with the Mini Nutritional Assessment (MNA), including weight, height, arm and calf circumference. Scores of 17–23.5 indicated “risk of malnutrition,” while scores <17 indicated “malnourished” [20].
To assess QoL, the EuroQol five-dimensional questionnaire (EQ-5D) was used, which includes five dimensions: Mobility, Self-care, Usual activities, Pain/discomfort, and Anxiety/depression. The instrument has three response levels, resulting in a five-digit code that is cross-referenced with the Brazilian QALY value table, with values from 0 (worst) to 1 (best QoL) [21].
Statistical analysis was performed with SPSS 25.0. Normality was tested with the Kolmogorov-Smirnov test. Descriptive analyses presented medians and interquartile ranges (P25 and P75) for nonparametric variables, and absolute or relative frequencies for categorical data.
The Mann-Whitney U test was used to compare medians between two nonparametric groups. Chi-square test was used for comparing proportions. Spearman’s correlation coefficient (ρ) was used for correlations, with significance set at p<0.05.
Multiple linear regression was performed with prerequisites: at least 20 subjects per independent variable, normally distributed residuals, absence of outliers, no multicollinearity, linear relationship between independent and dependent variables, and homoscedasticity. The Stepwise Backward method was used to develop the predictive model for QoL. The final model included unstandardized coefficients (B), regression coefficient (β), t-test, and p-values, indicating each variable’s contribution to the model
Results
Table 1 presents the sociodemographic and clinical characteristics of the sample.
Table 1 – Median values of the EQ-5D quality of life scores according to demographic and clinical variables of elderly women. Brasília, 2025
|
n |
Total |
EQ-5D Score |
|||||
|
% |
Median |
P25 |
P75 |
P Value |
|||
|
Age |
60 a 69 years |
85 |
32,9 |
0,690 |
0,590 |
0,780 |
0,648 |
|
70 a 79 years |
99 |
38,4 |
0,730 |
0,610 |
0,780 |
||
|
≥ 80 years |
74 |
28,7 |
0,695 |
0,610 |
0,750 |
||
|
Education |
Illiterate |
44 |
17,1 |
0,690 |
0,610 |
0,780 |
0,755 |
|
Elementary school |
137 |
53,1 |
0,730 |
0,610 |
0,780 |
||
|
High school |
55 |
21,3 |
0,705 |
0,610 |
0,780 |
||
|
Higher education |
22 |
8,5 |
0,730 |
0,610 |
0,800 |
||
|
Sedentary |
no |
104 |
40,3 |
0,730 |
0,610 |
0,780 |
0,411 |
|
yes |
154 |
59,7 |
0,685 |
0,600 |
0,780 |
||
|
Mental status |
normal |
244 |
94,6 |
0,710 |
0,610 |
0,780 |
0,973 |
|
Cognitive deficit |
14 |
5,4 |
0,695 |
0,610 |
0,730 |
||
|
Sarcopenia |
não |
206 |
79,8 |
0,730 |
0,630 |
0,800 |
0,038 |
|
yes |
52 |
20,2 |
0,690 |
0,610 |
0,780 |
||
|
Nutritional status |
Malnourished |
63 |
24,4 |
0,700 |
0,610 |
0,730 |
0,667 |
|
Eutrophic |
195 |
75,6 |
0,730 |
0,610 |
0,780 |
||
|
Constipacion |
no |
185 |
71,7 |
0,730 |
0,610 |
0,780 |
0,374 |
|
yes |
73 |
28,3 |
0,690 |
0,610 |
0,780 |
||
|
Edentulism |
no |
49 |
19,0 |
0,730 |
0,610 |
0,780 |
0,430 |
|
yes |
209 |
81,0 |
0,690 |
0,590 |
0,730 |
||
|
Dysfagia Risk |
no |
152 |
58,9 |
0,690 |
0,640 |
0,780 |
0,042 |
|
yes |
106 |
41,1 |
0,640 |
0,570 |
0,730 |
||
|
Polypharmacy |
no |
87 |
33,7 |
0,730 |
0,610 |
0,780 |
0,808 |
|
yes |
171 |
66,3 |
0,730 |
0,610 |
0,780 |
||
|
DM |
no |
147 |
57,0 |
0,730 |
0,610 |
0,780 |
0,268 |
|
yes |
111 |
43,0 |
0,690 |
0,610 |
0,730 |
||
|
HAS |
no |
48 |
18,6 |
0,730 |
0,610 |
0,790 |
0,403 |
|
yes |
210 |
81,4 |
0,695 |
0,610 |
0,780 |
||
|
Osteoporosis |
no |
156 |
60,5 |
0,730 |
0,610 |
0,800 |
0,024 |
|
yes |
102 |
39,5 |
0,690 |
0,610 |
0,730 |
||
|
Heart disease |
no |
217 |
84,1 |
0,720 |
0,610 |
0,780 |
0,880 |
|
yes |
41 |
15,9 |
0,690 |
0,610 |
0,780 |
||
|
IU |
no |
128 |
49,6 |
0,680 |
0,680 |
0,730 |
0,002 |
|
yes |
130 |
50,4 |
0,630 |
0,580 |
0,730 |
||
Legend: DM: diabetes mellitus; HTN: systemic arterial hypertension; UI: urinary incontinence.
Source: The authors.
Source: The authors.
Figure 2 - Median values of EQ-5D quality of life scores according to Sarcopenia. Brasília, 2025
Source: The authors.
Figure 3 - Median values of EQ-5D quality of life scores according to Risk of Dysphagia. Brasília, 2025
Regarding the evaluation of QoL dimensions, Pain/discomfort was the most affected (73.3%), followed by Anxiety/depression (72.9%). The Pain/discomfort dimension was associated with the risk of dysphagia (p < 0.001), and the Mobility dimension was associated with urinary incontinence (Table 2).
Table 2 – Association of EQ-5D quality of life dimensions in elderly women according to identified conditions. Brasília, 2025
|
EQ-5D Dimensions |
Total (n=258) |
Sarcopenia |
Risk of dysphagia |
Osteoporosis |
IU |
|
Pain/discomfort |
189 (73,3) |
46 (68,7) |
70 (66,0) * |
75 (73,5) |
92 (70,8) |
|
Anxiety/depression |
188 (72,9) |
49 (73,1) |
77 (72,6) |
69 (67,6) |
99 (76,2) |
|
Mobility |
76 (29,5) |
21 (31,3) |
26 (24,5) |
33 (32,4) |
30 (23,1) * |
|
Usual activities |
58 (22,5) |
16 (23,9) |
20 (18,9) |
21 (20,6) |
25 (19,2) |
|
Self-care |
8 (3,1) |
3 (4,5) |
2 (1,9) |
3 (2,9) |
3 (2,3) |
* p<0,001. Legend: UI: urinary incontinence.
Source: The authors.
The QoL prediction model showed no multicollinearity among the predictor variables, with standardized residuals within the normal range. Negative regression coefficients indicated a decrease in QoL. Thus, it was observed that dysphagia risk and UI significantly reduce the QoL of elderly women (Table 3).
Table 3 – Regression coefficients of the predictor variables for quality of life in elderly women included in the final model. Brasília, 2025
|
CNP |
CP |
|
|||
|
B |
Error |
Beta |
t |
P Value |
|
|
Sarcopenia |
-0,025 |
0,021 |
-0,071 |
-1,17 |
0,243 |
|
Rissk of dysfagia |
-0,057 |
0,019 |
-0,185 |
3,02 |
0,003 |
|
Osteoporosis |
0,036 |
0,019 |
0,115 |
1,927 |
0,055 |
|
IU |
-0,08 |
0,019 |
-0,264 |
-4,31 |
<0,001 |
Legend – B: unstandardized coefficient; Beta: standardized coefficient; UI: urinary incontinence.
Source: The authors.
Discussion
This study found worse QoL in elderly women with risk of dysphagia and urinary incontinence, although there was no maintained association with sarcopenia or osteoporosis, as previously observed in other studies conducted in Brazil [22]. The prevalence of sarcopenia in this sample was 20%, consistent with expectations for the Brazilian elderly population and findings from a systematic review [23]. The SABE study, by contrast, reported a lower prevalence of 4.8% [13].
Although no association was observed between sarcopenia and QoL in this study, the condition is known to be related to low muscle strength and reduced performance in activities of daily living. These factors influence the QoL dimensions of Mobility, Self-care, Usual activities, Pain, and Anxiety in the EQ-5D, as found in other research [24]. The lack of association may result from differences between QoL screening instruments [15].
Risk of dysphagia was present in nearly half of the sample, corroborating findings from a Danish study that highlighted how dysphagia negatively affects QoL, especially in psychological aspects. About one-third of participants in that study reported embarrassment when eating in public, sadness over not finishing meals, and inability to enjoy eating as before—feelings of disability or limitation were common [25]. Another study identified dysphagia risk in 37.27% of elderly individuals, with swallowing difficulty becoming a burden from age 70 onward. The worst QoL scores were found in the Sleep and Fatigue domains of the SWAL-QOL scale [26].
Professional assessment using validated tools is crucial for identifying dysphagia early. A study in Japan reported dysphagia prevalence between 25% and 54% in elderly people, with higher rates among the frail and dependent [27]. A literature review also found strong evidence of dysphagia’s prevalence in the elderly and emphasized the need for multidisciplinary intervention to prevent complications [12].
This study found a correlation between dysphagia risk and the Pain/discomfort dimension, indicating pain or discomfort while eating. This can lead to reduced food quality and quantity, food exclusion, and altered meal consistency. A quarter of the sample was malnourished, suggesting elderly women are at higher nutritional risk than the general population. Although this study found a relationship between dysphagia and QoL, comparisons with other studies are limited due to the use of different instruments—e.g., EQ-5D does not include Sleep and Fatigue domains [24].
In cases of unhealthy or inadequate aging, physical-functional decline may occur, directly contributing to disability and low QoL. Notably, there was a high prevalence of edentulism in this sample. Oral health is associated with ADLs, muscle mass, and nutritional status. Oral problems, such as tooth loss, are linked to malnutrition, dysphagia, and sarcopenia. Poor oral health may also trigger systemic inflammation, which affects physical performance, especially muscle mass, strength, and function. Swallowing or chewing issues can result in poor food intake, weight loss, and development of malnutrition, sarcopenia, and frailty [28].
The high prevalence of urinary incontinence (UI) in this study confirms it as a predominantly female issue. A study in Marília–São Paulo found even higher UI prevalence, which significantly affected the population’s QoL [29]. Another Brazilian study reported 36.32% UI in women, with moderate QoL impact [30]. Negative impacts of UI on elderly women’s QoL were also confirmed in a study where UI was described as unpleasant and stressful, causing a loss of control, shame, discomfort, insecurity, suffering, and guilt. It negatively influenced physical, social, sexual, and autonomy domains [31].
Literature suggests that UI can be associated with sarcopenia due to reduced muscle mass and strength, especially in abdominal and pelvic floor muscles, which play important roles in stress and urgency UI pathophysiology. Pelvic floor strength is key to preventing both stress and urge incontinence. Since sarcopenia affects skeletal muscles, including the pelvic floor and abdominal muscles, it may increase susceptibility to UI [32].
Specifically, UI showed a significant relationship with the Mobility dimension of EQ-5D, consistent with studies conducted in Korea and Australia. The Korean study, with a large and diverse sample, found associations between UI and Mobility, Usual activities, Pain/discomfort, and Anxiety/depression [33]. The Australian multicenter study also found significant association between UI and Mobility, indicating greater QoL impact with more severe UI. It recommended interventions to preserve or restore mobility to minimize or prevent UI in geriatric populations [34].
UI can cause discomfort, social isolation, and low self-esteem in women, significantly harming their QoL. One study found that 81.82% of women reported UI negatively affected their QoL [35].
The results of this study underscore the need for further investigation into the association between dysphagia risk, UI, and poor QoL. Additional research should explore factors related to sarcopenia and dysphagia in different elderly populations.
The findings suggest that sarcopenia and dysphagia risk impair QoL, and this topic requires more attention. There is a need to develop public policies and care pathways and to evaluate the impact on QoL among populations with neurodegenerative and/or neurological diseases that may develop sarcopenia and dysphagia secondarily. The use of validated, easy-to-apply screening tools for dysphagia, UI, sarcopenia, and malnutrition is essential to guide the creation of specific outpatient services that can reduce the consequences for elderly populations.
This study is limited by its cross-sectional design, which prevents establishing cause-effect relationships, and by being conducted in a reference unit, limiting generalizability.
It is believed that the earlier clinical conditions such as malnutrition, dysphagia, sarcopenia, and QoL impairment are screened and diagnosed, the sooner interventions at the primary and secondary levels of elderly healthcare can be implemented—minimizing hospitalization risks and reducing costs. The overlap of these health conditions may support the development of interprofessional teams in geriatrics and gerontology
Conclusion
The results showed that elderly women at risk of dysphagia and with urinary incontinence presented lower QoL scores, especially in the Pain/discomfort and Mobility dimensions. No association was observed between sarcopenia and QoL. Monitoring elderly women at risk of dysphagia and sarcopenia is recommended to promote better quality of life.
Acknowledgments
To the Research Promotion Program of the Higher School of Health Sciences (ESCS) and the Foundation for Teaching and Research in Health Sciences (FEPECS).
Conflict of interest
The authors declare no conflict of interest.
Funding sources
This research was funded by the Research Promotion Program of the School of Health Sciences, with resources from the Foundation for Teaching and Research in Health Sciences. TOA 05/2023.
Author contributions
Conception and design of the study: Cerceau VR, Pinheiro HA, Stival MM; Data collection: Cerceau VR; Data analysis and interpretation: Cerceau VR, Stival MM; Manuscript writing: Cerceau VR, Silva MC; Critical review of the manuscript for important intellectual content: Cerceau VR, Pinheiro HA, Stival MM.
References
1. World Population Prospects 2019: Highlights United Nations- New York, 2019. Disponível em: HYPERLINK “https://bristoluniversitypressdigital.com/edcollchap/book/9781447356127/ch007.xml”https://bristoluniversitypressdigital.com/edcollchap/book/9781447356127/ch007.xml doi: HYPERLINK “https://doi.org/10.51952/9781447356127.ch007”https://doi.org/10.51952/9781447356127.ch007.
2. Atenção Integrada para os Idosos (ICOPE): Atenção integrada para os idosos. Orientações sobre a avaliação centrada na pessoa e roteiros para a atenção primária, Washington. D.C.: OPAS, -1, 2020. Disponível em: https://iris.paho.org/handle/10665.2/51974%202020
3. Ferraz MST, Guimarães MF, Nunes JA, et al. Risco de Disfagia e Qualidade de Vida em Idosos Saudáveis. Distúrb Comun [Internet]. 2020;32(3):454-61. Disponível em: https://revistas.pucsp.br/index.php/dic/article/view/44540. doi: https://doi.org/10.23925/2176-2724.2020v32i3p454-461.
4. Cruz-Jentoft AJ, Bahat G, Bauer J, et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing,Oxford, 2019; 48(1):16–31. Disponível em: https://academic.oup.com/ageing/article/48/1/16/5126243?login=false. doi: https://doi.org/10.1093/ageing/afy169
5. Diz JBM, Leopoldino AAO, Moreira BDS, et al. Prevalence of sarcopenia in older Brazilians: A systematic review and meta-analysis. Geriatr Gerontol Int. 2017;17(1)5–16. Disponível em: https://onlinelibrary.wiley.com/doi/abs/10.1111/ggi.12720. doi: https://doi.org/10.1111/ggi.12720.
6. Da Silva MM, de Araújo MG, da Silva AM, Gonçalves DL, da Silva KF, Medeiros LGC, et al. Prevalência de sarcopenia em idosos brasileiros: uma revisão bibliográfica. BRASPEN Journal.2023;36(3):14-322. Disponível em: https://braspenjournal.org/article/doi/10.37111/braspenj.2021.36.3.13 doi: http://dx.doi.org/10.37111/braspenj.2021.36.3.13.
7. Darvishi A, Shafiee G, Balajam NZ, Hemami MR, Ostovar N, Heshmat R. Cost - effectiveness analysis of sarcopenia management interventions in Iran. BMC Public Health.2023;1–14. Disponível em: https://link.springer.com/article/10.1186/s12889-023-15693-w doi: https://doi.org/10.1186/s12889-023-15693-w
8. Fujishima I, Fujiu-Kurachi M, Arai H, et al. Sarcopenia and dysphagia: Position paper by four professional organizations. Geriatr Gerontol Int. 2019;19(2):91–7. Disponível em: https://onlinelibrary.wiley.com/doi/full/10.1111/ggi.13591 doi: https://doi.org/10.1111/ggi.13591
9. De Sire A, Ferrillo M, Lippi L, et al. Elderly: A Comprehensive Review, Nutrients.2022;14(5):982. Disponível em: https://www.mdpi.com/2072-6643/14/5/982. doi: https://doi.org/10.3390/nu14050982
10. Cuppari, L. Nutrição Clínica no Adulto. 4. ed.: Manole. 2019. São Paulo;624.
11. Budni CSJ. The dysphagia in the aging associated with mental disorder and malnutrition., periódicos.unesc.net. 2019;9(1):142. Disponivel em: https://www.periodicos.unesc.net/ojs/index.php/Inovasaude/article/view/3588. doi: https://doi.org/10.18616/inova.v9i1.3588
12. Benzecry G, da Silva BP, Foliene AC, et al. Prevalência E Fatores Associados Dysphagia in Elderly : a Review. Disciplinarum Scientia. Série: Ciências da Saúde, Revista Inova Saúde, Santa Maria. 2020;21(2):1-10. Disponível em: https://periodicos.ufn.edu.br/index.php/disciplinarumS/article/view/3045 doi: https://doi.org/10.37777/dscs.v21n1-024
13. Alexandre T da S, Duarte YADO, Santos JLF, et al. Prevalence and associated factors of sarcopenia, dynapenia, and sarcodynapenia in community-dwelling elderly in São Paulo – sabe study. Rev Bras Epidemiol,Sao Paulo. 2018;21 Suppl 2:1–13. Disponível em: https://www.scielo.br/j/rbepid/a/rdHTbFf4RCCSkQm5zMWhPgw/?lang=en. doi: https://doi.org/10.1590/1980-549720180009.supl.2 .
14. Wróblewska Z, Chmielewski JP, Wojciechowska M, et al. Evaluation of the quality of life of older people with diabetes. Ann Agric Environ Med, 2023;30(3):505-512. Disponível em: https://pubmed.ncbi.nlm.nih.gov/37772527/ doi: https://doi.org/10.26444/aaem/168415.
15. Tsekoura M, Kastrinis A, Katsoulaki M, et al. Sarcopenia and Its Impact on Quality of Life. Quality of Life. GeNeDis. 2017;213–8. Disponível em: https://link.springer.com/chapter/10.1007/978-3-319-57379-3_19. doi: https://doi.org/10.1007/978-3-319-57379-3_19.
16. Melo DM. De, Barbosa AJG. O uso do Mini-Exame do Estado Mental em pesquisas com idosos no Brasil: uma revisão sistemática. Ciência & Saúde Coletiva, [s. l.]2015; 20(12):3865–3876. Disponível em: https://doi.org/10.1590/1413-812320152012.06032015 doi: https://doi.org/10.1590/1413-812320152012.06032015.
17. Pereira AVN, Santos LD, Pedreira RBS, et al. Prevalence and factors associated with dynapenia in older women using different diagnostic criteria. Motriz: Revista de Educação Física, [s. l.],2022;28. Disponível em: https://doi.org/10.1590/s1980-657420220005822. doi: https://doi.org/10.1590/s1980-657420220005822 .
18. Kim KM, Jan HC, Lim S. Differences among skeletal muscle mass indices derived from height-, weight-, and body mass index-adjusted models in assessing sarcopenia. Korean Journal of Internal Medicine,2016;31(4):643–50. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4939509/. doi: https://doi.org/ 10.3904/kjim.2016.015.
19. Gonçalves MIR, Remaili CB, Behlau M. Cross-cultural adaptation of the Brazilian version of the Eating Assessment Tool - EAT-10. Codas.2013;25(6):601–4. Disponível em: https://www.scielo.br/j/codas/a/QYqVrkLzCxDbZmdCVhwxSyK/?lang=en.doi: https://doi.org/10.1590/S2317-17822013.05000012 .
20. Campos JO, Carvalho MF, Leite AFB. Utilização da mini avaliação nutricional em visitas domiciliares na atenção primária a saúde. J Meml da Med, 2020;2(1):20-25. Dispinível em: https://www.jornalmemorialdamedicina.com/index.php/jmm/article/view/27 .doi : https://doi.org/10.37085/jmmv2.n1.2020.pp.20-25.
21. Santos M, Monteiro AL, Santos B. EQ 5D Brazilian population norms. Health Qual Life Outcomes. 2021;19(1):162. Disponível em: https://link.springer.com/article/10.1186/s12955-021-01671-6. doi: https://doi.org/10.1186/s12955-021-01671-6.
22. Chagas CS, Ohara DG. Associação entre sarcopenia e qualidade de vida relacionada à saúde em idosos comunitários. Acta Paul. Enferm. (Online), v.34, n.1, eAPE002125, 2021. Disponível em: https://www.scielo.br/j/ape/a/ZwK5b9yVkc5sNP4xQCypDpB/. doi: https://doi.org/10.37689/acta-ape/2021AO002125.
23. da Silva MM, de Araújo MG, da Silva AM, Gonçalves DL, da Silva KF, Medeiros LGC. Prevalência de sarcopenia em idosos brasileiros: uma revisão bibliográfica. BRASPEN Journal.2023;36(3):14-322. Disponível em: https://braspenjournal.org/article/doi/10.37111/braspenj.2021.36.3.13 doi: http://dx.doi.org/10.37111/braspenj.2021.36.3.13.
24. Silva Neto LS, Karnikowski MG, Osório NB, et al. Association between sarcopenia and quality of life in quilombola elderly in Brazil. Int J Gen Med.2016;9:89–97. Disponível em: https://www.tandfonline.com/doi/full/10.2147/IJGM.S92404. doi:https://doi.org/10.2147/IJGM.S92404.
25. Bendsen BB, Jensen D, Westmark S, et al. The Quality of Life in Citizens with Oropharyngeal Dysphagia — A Cross-Sectional Study. J. Clin. Med.2022;11(14):4212. Disponível em: https://www.mdpi.com/2077-0383/11/14/4212. doi:. https://doi.org/10.3390/jcm11144212.
26. Ferraz MST, Guimarães MF, de Alencar Nunes J, Azevedo EHM. Risco de Disfagia e Qualidade de Vida em Idosos Saudáveis. Distúrb Comun, São Paulo, v.32, n.3, p.454-61, 2020. Disponível em: https://revistas.pucsp.br/index.php/dic/article/view/44540. doi: https://doi.org/10.23925/2176-2724.2020v32i3p454-461.
27. Igarashi K.; Kikutani T.; Tamura F. Survey of suspected dysphagia prevalence in home-dwelling older people using the 10-Item Eating Assessment Tool (EAT-10). PLoS One, v.14, n.1, 2019. Disponível em: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0211040. doi: https://doi.org/10.1371/journal.pone.0211040.
28. Bayram HM, Ilgaz F, Serel Arsla S, Demir N, & Rakıcıoğlu N. The relationship between dysphagia, oral health, masticatory performance and activities of daily living in elderly individuals as assessed by the Eating Assessment Tool. Prog Nutr.2021;23(1):1-8. Disponível em: https://hdl.handle.net/11363/4956. doi: https://doi.org/ 10.23751/pn.v23i1.9101.
29. Evangelista DR, Gazetta FADA, Assis LC. Prevalência de incontinência urinária em idosas e impacto na qualidade de vida/ Prevalence of urinary incontinence in elderly women and impact on quality of life. Braz. J. Hea. Rev. [Internet].2021;4(1):1588-602. Disponível em: https://ojs.brazilianjournals.com.br/ojs/index.php/BJHR/article/view/23462 doi: https://doi.org/10.34119/bjhrv4n1-133.
30. Alves CA,Ferreira DCC, Lima MFD, Coimbra KA,Vaz CT. Prevalence of urinary incontinence, impact on quality of life and associated factors in users of Primary Health Care Units. Fisioter. Mov.2022;35. Disponível em: https://www.scielo.br/j/fm/a/HNXYbgWNkCjzkWmsQSDhryG/. doi: https://doi.org/10.1590/fm.2022.35604.
31. Oliveira LGP, Tavares ATDVB, Amorim TV, et al. Impacto da incontinência urinária na qualidade de vida de mulheres: revisão integrativa da literatura. Rev enferm UERJ.2020;28:e51896. Disponível em: https://www.e-publicacoes.uerj.br/enfermagemuerj/article/view/51896. doi: http://dx.doi.org/10.12957/reuerj.2020.51896.
32. Erdogan T, Bahat G, Kilic C, Kucukdagli P, Oren MM, Erdogan O et al. The relationship between sarcopenia and urinary incontinence. European Geriatric Medicine.2019;10(6): 923-929. Disponível em: https://link.springer.com/article/10.1007/s41999-019-00232-x. doi: https://doi.org/10.1007/s41999-019-00232-x.
33. Kwon CS, Lee JH. Prevalence, Risk Factors, Quality of Life, and Health-Care Seeking Behaviors of Female Urinary Incontinence: Results From the 4th National Health and Nutrition Examination Survey VI (2007-2009). Int Neurourolj.2014;18(1):31-6.Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3983507/. doi: https://doi.org/10.12957/reuerj.2020.51896.
34. Jachan DE, Müller-Werdan U, Lahmann NA. Impaired Mobility and Urinary Incontinence in Nursing Home Residents A Multicenter Study. A Multicenter Study. J Wound Ostomy Continence Nurs.2019;46(6):524-9. Disponível em: https://journals.lww.com/jwocnonline/abstract/2019/11000/impaired_mobility_and_urinary_incontinence_in.9.aspx. doi: https://doi.org/ 10.1097/WON.0000000000000580.
35. Silva JVB. Prevalência de mulheres com incontinência urinária e seu impacto na qualidade de vida. Revista Baiana de Saúde Pública.2024;48(1):91-101. Disponível em: https://pesquisa.bvsalud.org/portal/resource/pt/biblio-1555774. doi: https://doi.org/10.22278/2318-2660.2024.v48.n1.a3971.